About the Microbiome
THE MICROBIOME
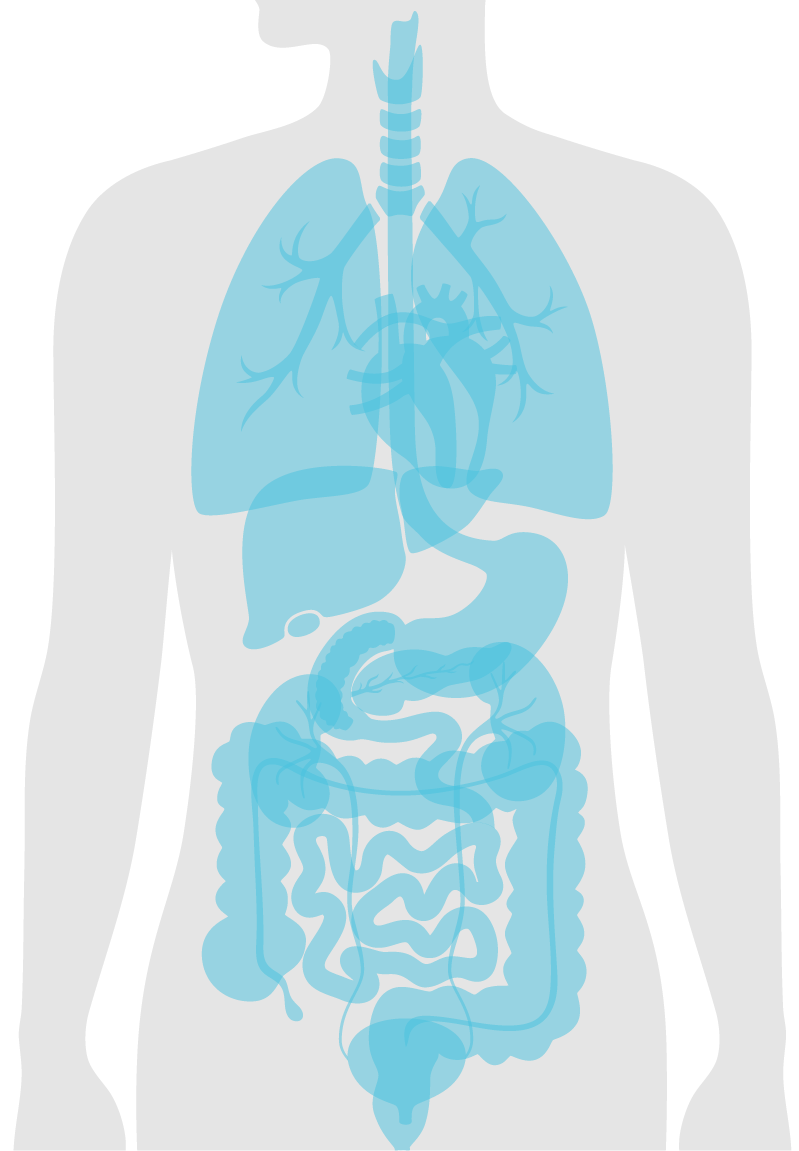
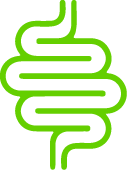
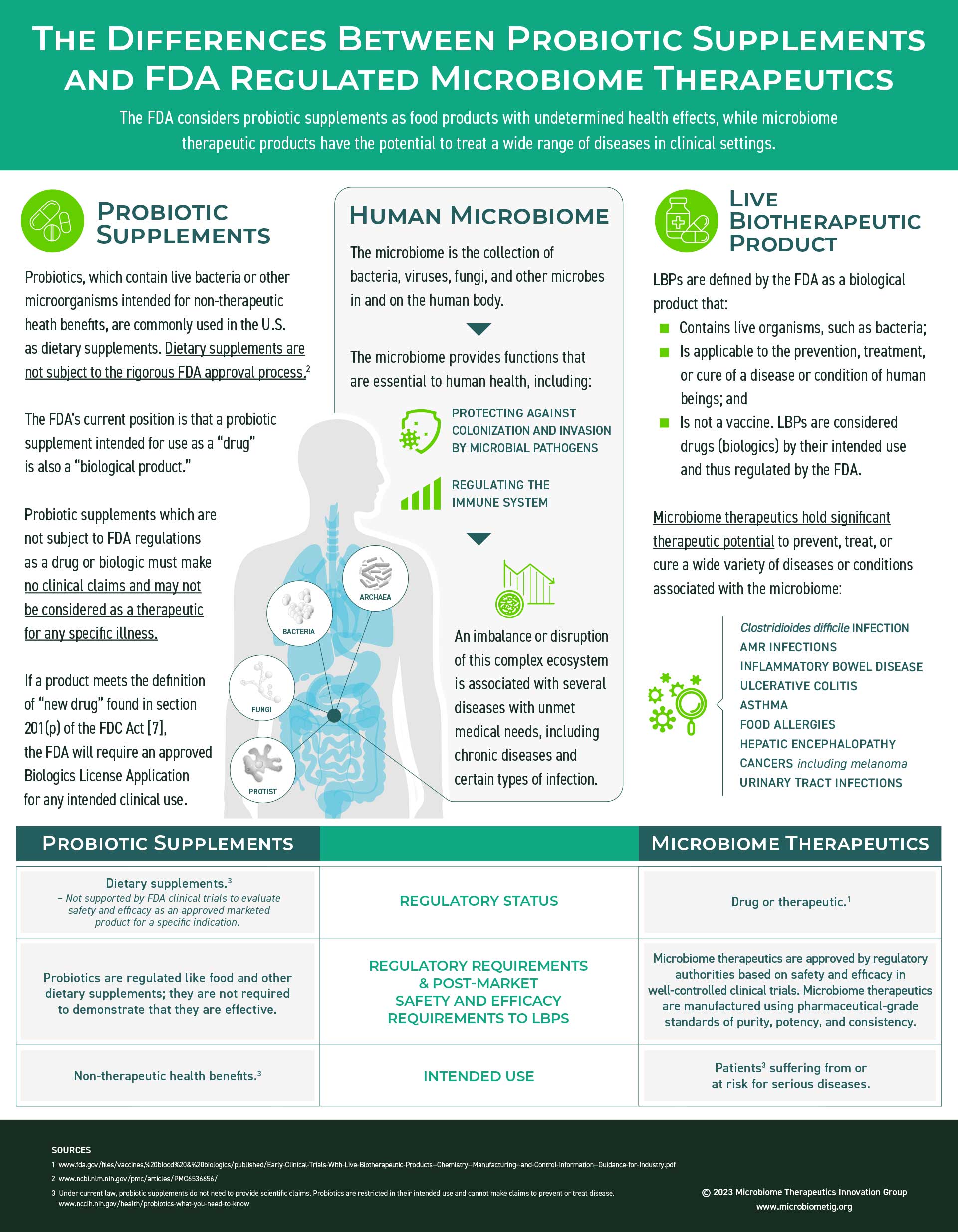
The human microbiome provides metabolic and synthetic functions essential to the human health, including regulating the immune system and aiding in digestion. It also provides protection against colonization and invasion by potential microbial pathogens. Through a complex network of interacting microbes, the microbiome directly or indirectly affects physiologic and immunologic functions. An imbalance or disruption of this complex ecologic system can lead to “dysbiosis”, which is characterized by a loss of microbial diversity and is now associated with a multitude of chronic diseases and some infections.
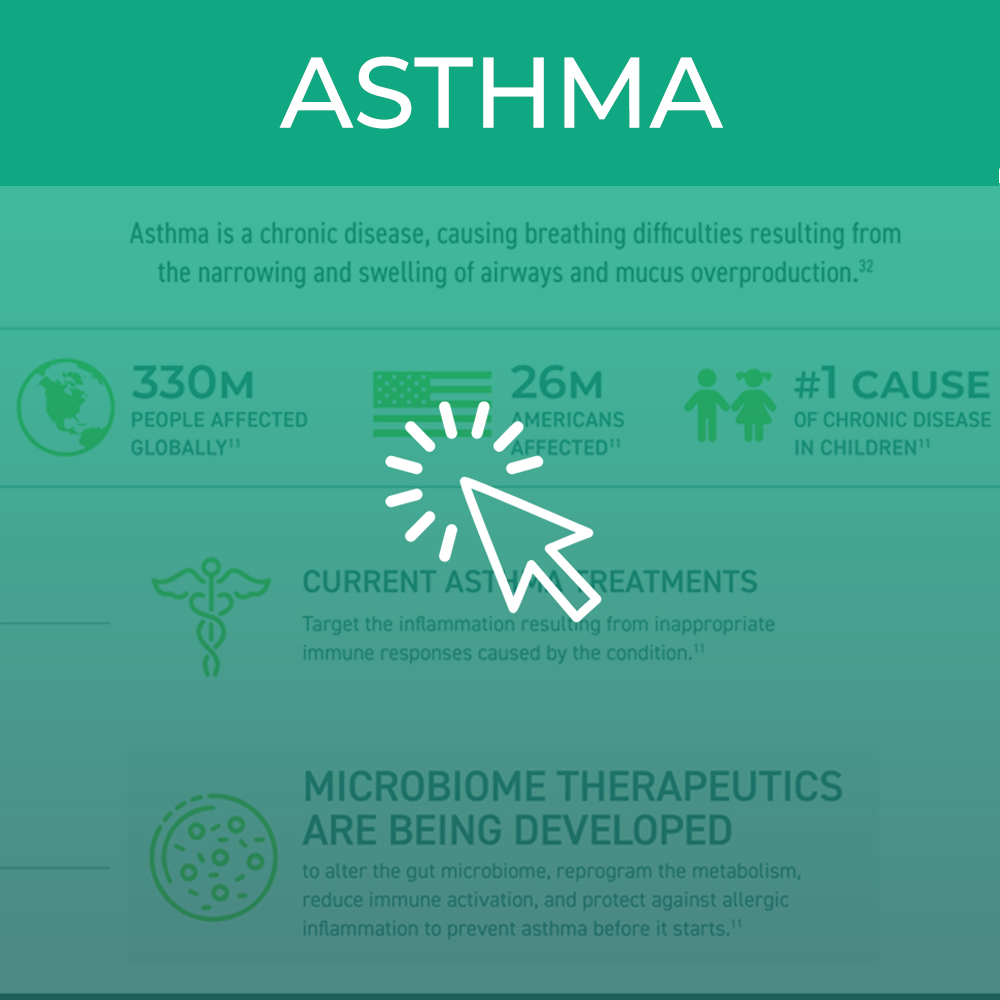
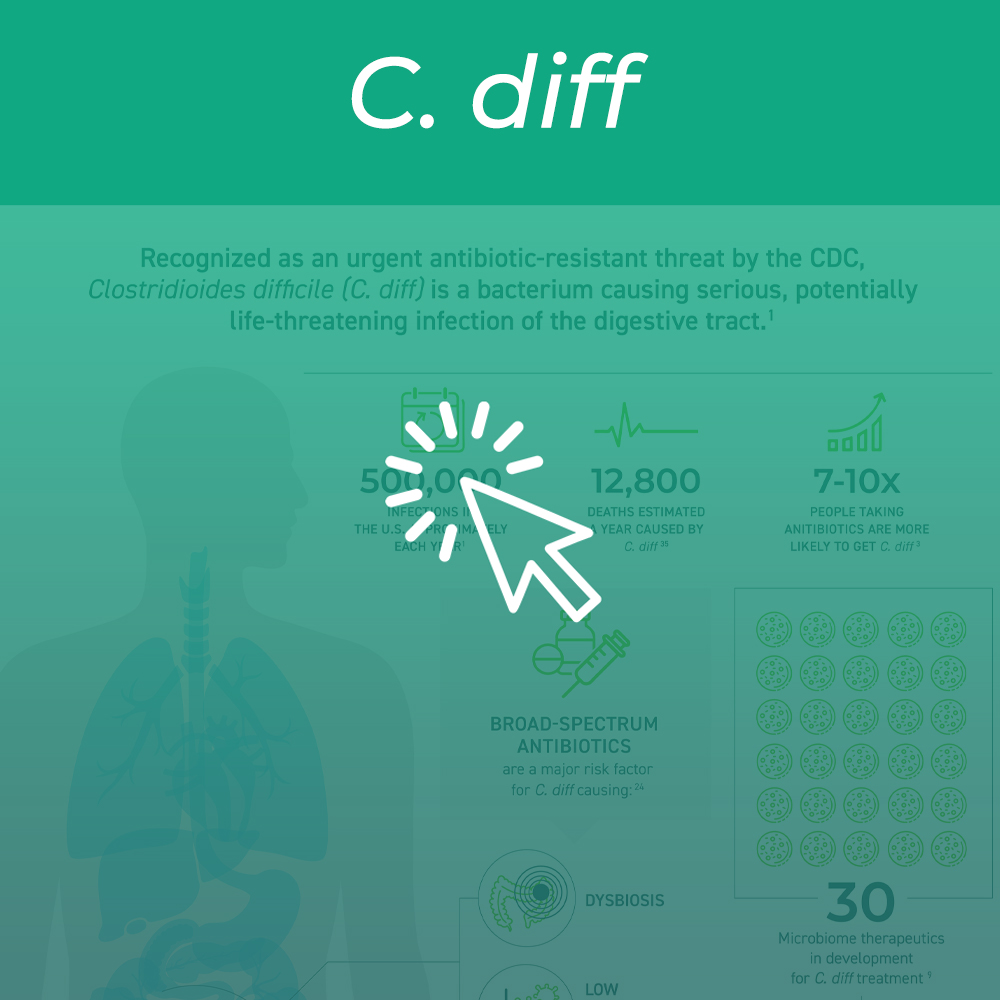
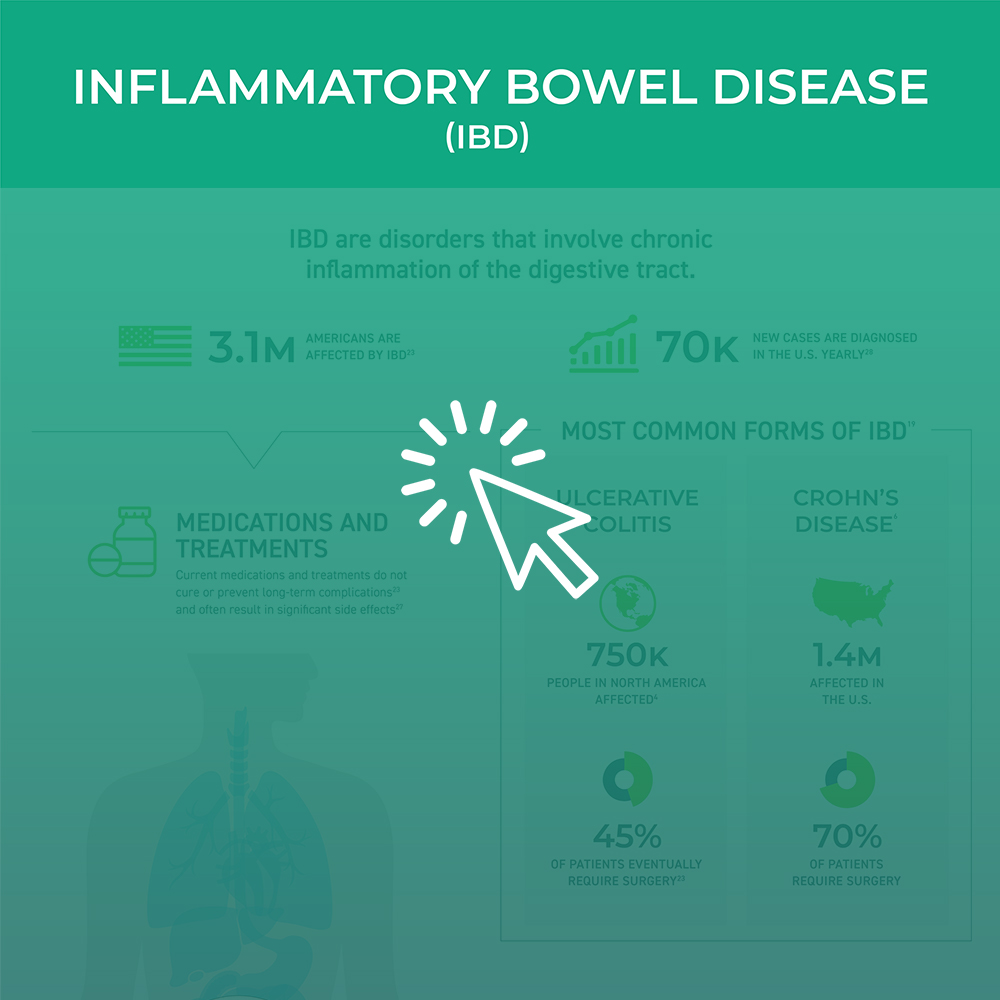
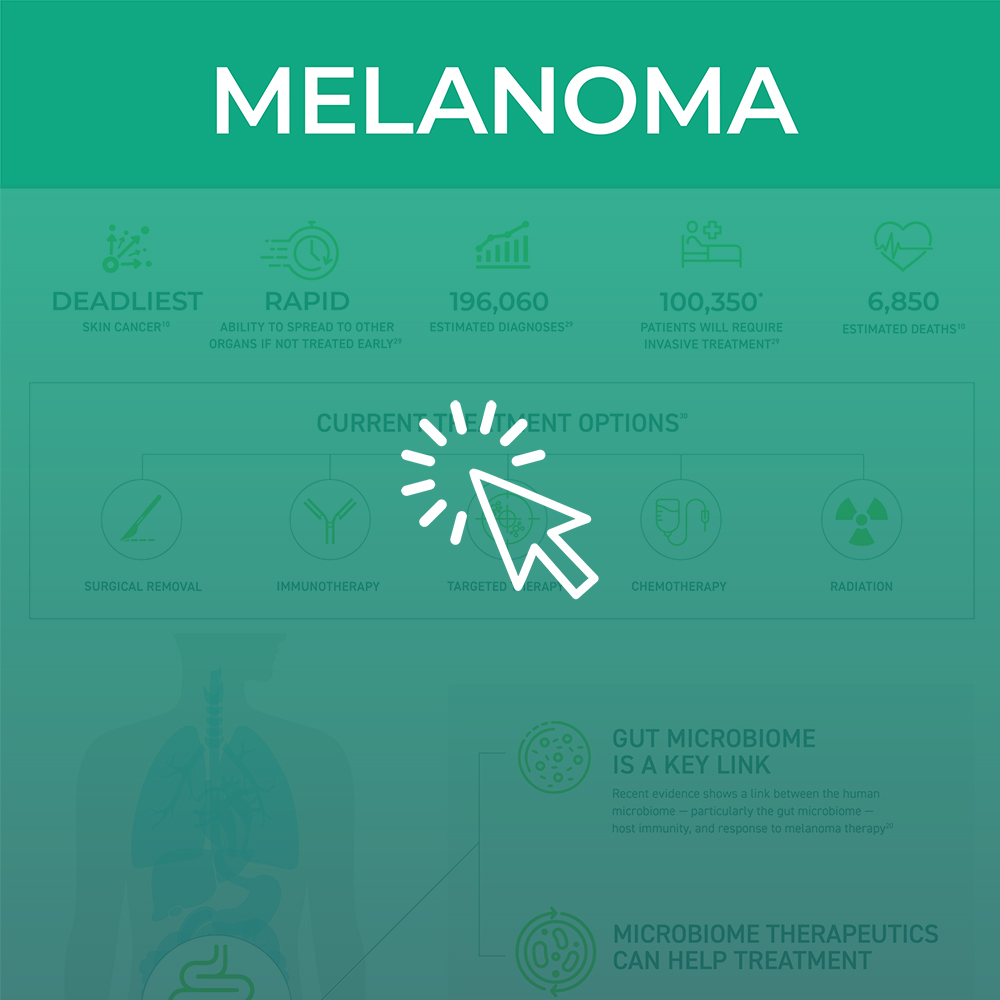
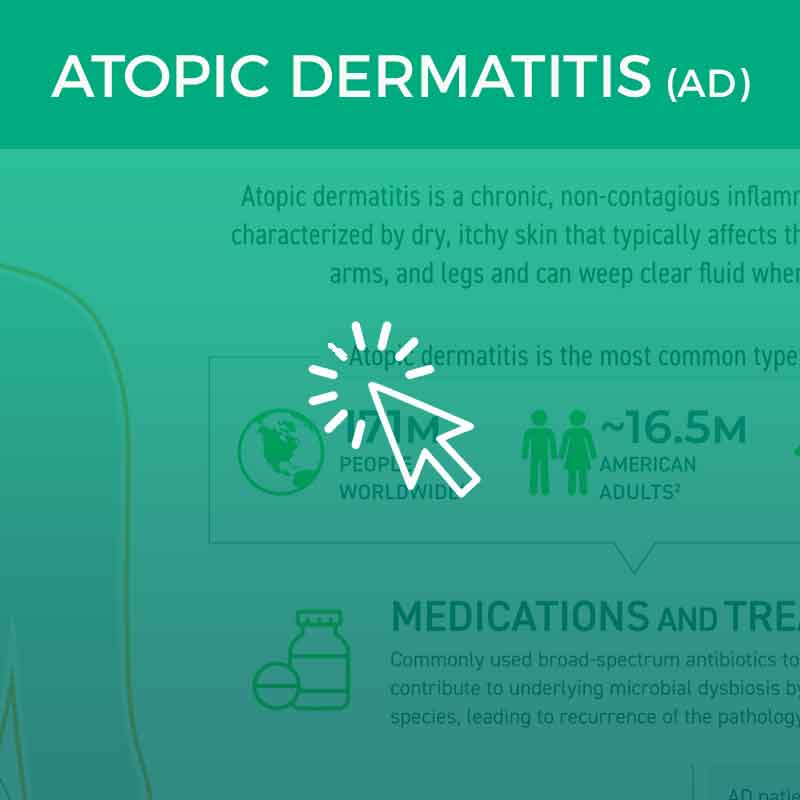
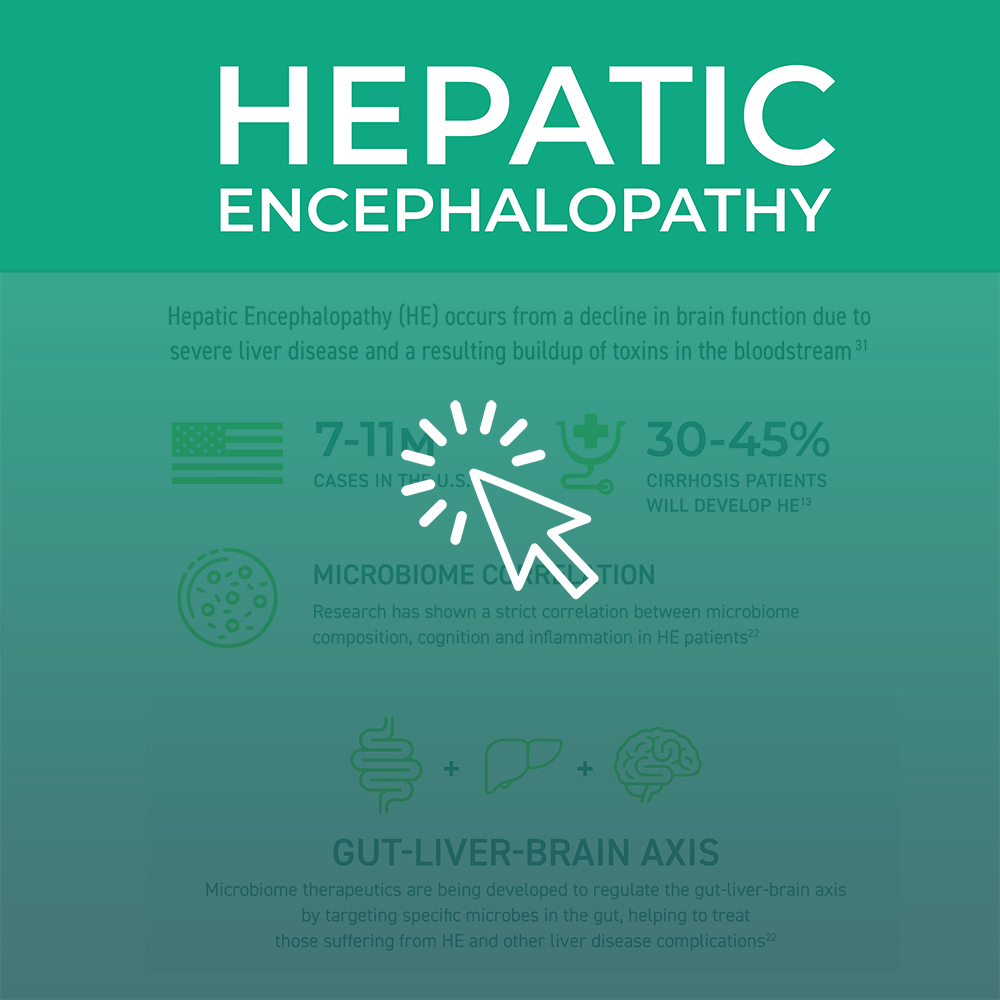
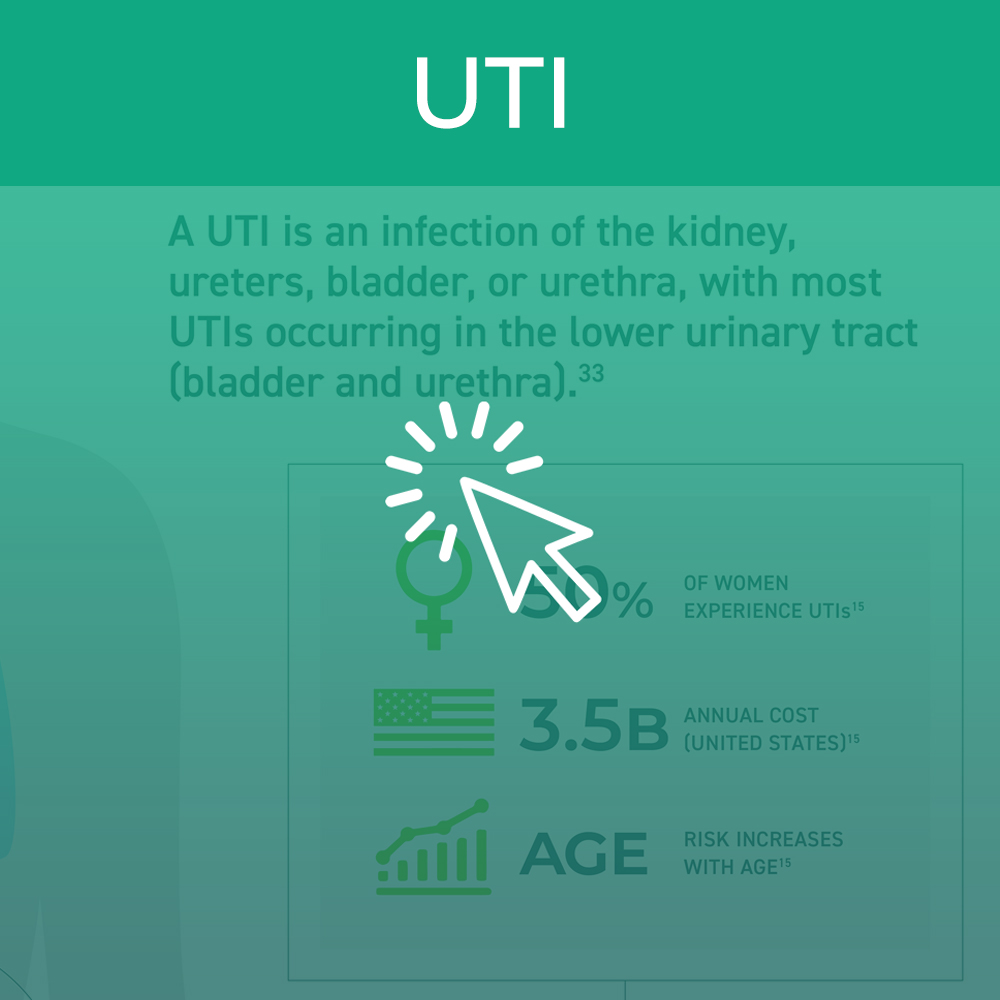
Improvement of dysbiosis through microbiome therapeutics is an exciting new frontier for medical innovation. The area of research that is best understood at present is the important role the microbiome plays in preventing recurrent Clostridium difficile infection (CDI). Dysbiosis secondary to antibiotic exposure leads to vulnerability to CDI with recurrent disease occurring in a significant subset of patients. Emerging data also support a key role of dysbiosis in inflammatory bowel disease (IBD) and other intestinal disorders such as irritable bowel syndrome (IBS), coeliac disease, and colon cancer. In fact, the role of the microbiome is now perceived to be so influential to human health that a multitude of other disorders are being explored such as allergy, asthma, metabolic syndrome, cardiovascular disease and liver disease. Finally, recognition of a potential connection of dysbiosis through the gut-brain microbiome axis has led to interest in assessing the potential role of microbiome therapeutics in neurodegenerative diseases like Alzheimer’s and Parkinson’s. Other areas of discovery in microbiome research include women’s health (bacterial vaginosis), oral medicine (dental carries), pulmonary (cystic fibrosis) and dermatology (acne).
The unmet medical needs are substantial. The Centers for Disease Control and Prevention (CDC) estimates that 1.4 million Americans suffer from IBD, yet only a third of them respond to existing therapies. Preliminary data from microbiome therapy suggest that improvement in dysbiosis is associated with a clinical response and remission in patients with ulcerative colitis, a form of chronic IBD. Microbiome therapeutics have the potential to serve as a bridge to stabilize disease flares and delay the need for chronic immunosuppressive therapies. The CDC also recognizes C. difficile as one of the top three urgent bacterial threats in the US affecting more than 450,000 persons/year. Yet one of every four persons relapses after standard of care antibiotics, which do not kill the dormant spores that germinate in the setting of persistent dysbiosis. However, disruption of dysbiosis is associated with resolution of relapsing infection. While studies of the gut microbiome have dominated research and clinical studies, the therapeutic potential of the microbiome in other body sites is also vast. Therefore, coalition efforts will embrace a broad scope of interests.
FDA-approved Microbiome Therapeutics (MT) have vast potential to help treat a wide range of diseases and conditions across gastrointestinal, neurological, immunological, oncological, and other indications. The field has grown exponentially in the past several years including the FDA approval of the first two microbiota-based products.
MICROBIOME THERAPEUTICS APPLICATIONS
MICROBIOME THERAPEUTICS APPLICATIONS
CROHN’S DISEASE
C. DIFFICILE
INFLAMMATORY BOWEL DISEASE
ULCERATIVE COLITIS
URINARY TRACT INFECTIONS
CANCER
ALLERGIC DISEASES
METABOLIC DISEASES
ATOPIC DERMATITIS
LIVER DISEASE COMPLICATIONS
DIABETES
ALZHEIMER’S DISEASE

MTIG is a coalition of companies leading the research and development of FDA-approved microbiome therapeutics and microbiome-based products to:
IMPROVE CLINICAL OUTCOMES
& QUALITY OF LIFE
ADDRESS UNMET
MEDICAL NEEDS
REDUCE HEALTH
CARE COSTS
MTIG is committed to working with stakeholders to collaborate with patients, healthcare providers, organizations, policymakers, and others who seek tangible policy and regulatory solutions to issues in the emerging microbiome arena.
SOURCES
- www.sciencealert.com/how-many-bacteria-cells-outnumber-human-cells-microbiome-science
- www.britannica.com/science/human-microbiome
- depts.washington.edu/ceeh/downloads/FF_Microbiome.pdf
- microbiometig.org/about-the-microbiome/
- www.microbiometimes.com/the-microbiome-biotech-landscape-an-analysis-of-the-pharmaceutical-pipeline/
- www.grandviewresearch.com/press-release/global-microbiome-therapeutics-market
- www.microbiometimes.com/drug-database-2/